Deaths from drug-resistant infections are set to skyrocket by 2050, according to the UN 2023 report ‘Bracing for Superbugs: Strengthening environmental action in the One Health response to antimicrobial resistance.’ Unless drastic action is taken to tackle the problem, it could also lead to a GDP shortfall of $3.4 trillion annually in the next decade and push 24 million more people into extreme poverty.
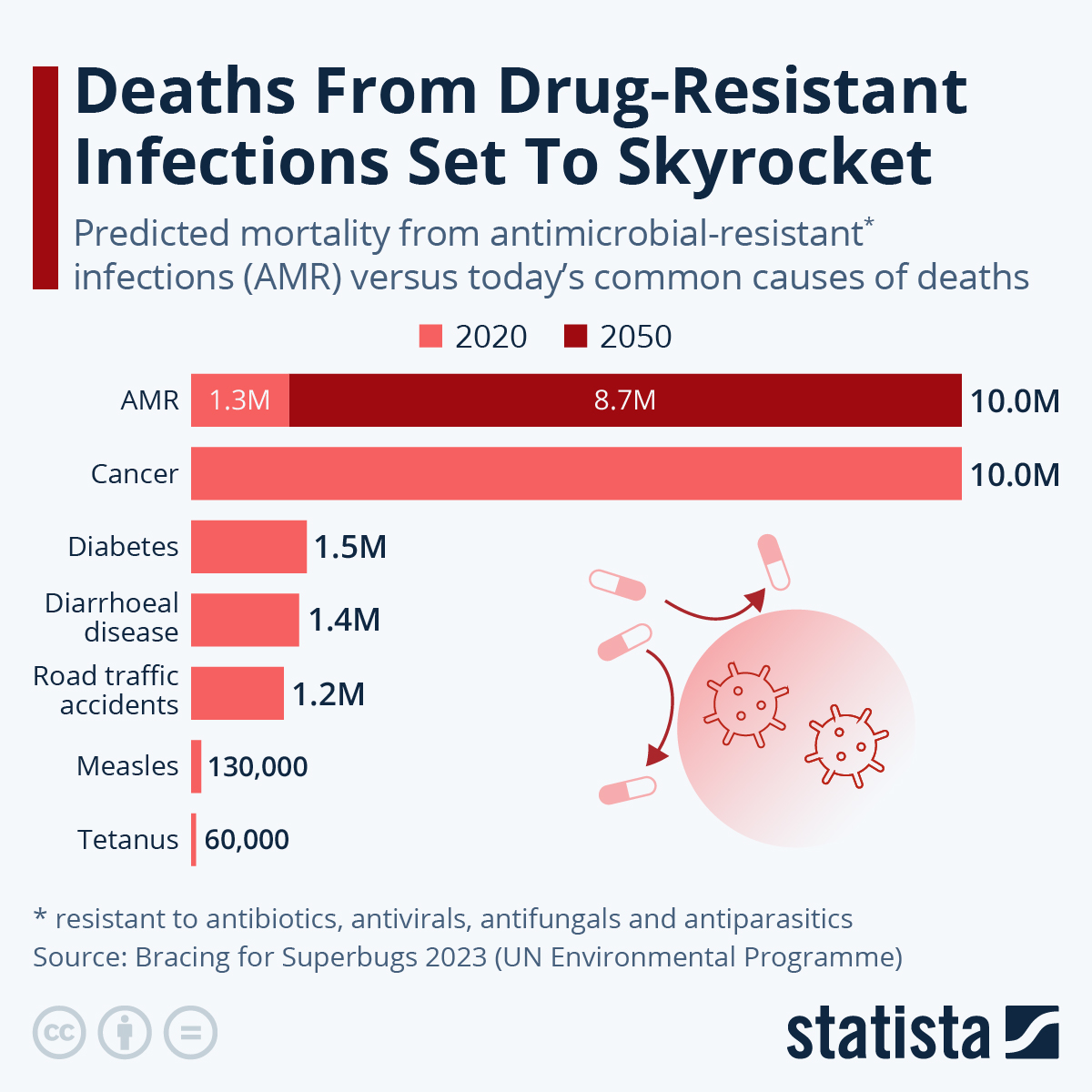
According to recent estimates, in 2019, 1.27 million deaths were directly attributed to drug-resistant infections globally, while 4.95 million deaths were linked with bacterial AMR. That’s now well above the death counts of major killers HIV/AIDS and malaria, which were estimated to have claimed the lives of 860,000 and 640,000, respectively, that year. As the following chart shows, antibiotic-resistant infections could kill as many as 10 million people in just three decades - on par with the 2020 death toll from cancer.
Although the risks of AMR will impact people worldwide, Low-Income Countries (LICs) and Lower-Middle-Income Countries (LMICs) are expected to see the highest death tolls. By region, Asia is predicted to see the highest number of AMR-related deaths per 10,000 population in 2050 (4,730,000), followed by Africa (4,150,000), Latin America (392,000), Europe (390,000), North America (317,000) and Oceania (22,000).
According to the report, AMR also exacerbates inequalities within societies and so groups including women, children, migrants, refugees, people employed in sectors such as agriculture or healthcare, as well as those living in poverty will be particularly vulnerable to drug-resistant infections.
Source: https://www.statista.com